MEDIZIN
AWARDS
Forschergeist gefragt: 14. Novartis Oppenheim-Förderpreis für MS-Forschung ausgelobt
FernstudiumCheck Award: Deutschlands beliebteste Fernhochschule bleibt die SRH Fernhochschule
Vergabe der Wissenschaftspreise der Deutschen Hochdruckliga und der Deutschen Hypertoniestiftung
Den Patientenwillen auf der Intensivstation im Blick: Dr. Anna-Henrikje Seidlein…
Wissenschaft mit Auszeichnung: Herausragende Nachwuchsforscher auf der Jahrestagung der Deutschen…
VERANSTALTUNGEN
Wichtigster Kongress für Lungen- und Beatmungsmedizin ist erfolgreich gestartet
Virtuelle DGHO-Frühjahrstagungsreihe am 22.03. / 29.03. / 26.04.2023: Herausforderungen in…
Pneumologie-Kongress vom 29. März bis 1. April im Congress Center…
Die Hot Topics der Hirnforschung auf dem DGKN-Kongress für Klinische…
Deutscher Schmerz- und Palliativtag 2023 startet am 14.3.
DOC-CHECK LOGIN
Comprehensive Care – difference and common aspects of acute treatment and chronic care
From Prof. Dr. Ley Sander, London, UK
Berlin (20. September 2008) – Epilepsy is the most common serious neurological disorder with a lifetime prevalence of between two and five percent. Many of those developing epilepsy do so at a young age. The prevalence of active epilepsy (ie people with ongoing seizures) is up to one percent of the general population. For many people who develop epilepsy, the condition is short lived, but in about one fifth of those who develop epilepsy the condition becomes chronic with little prospect for full seizure remission.
Having recurrent epileptic seizures has implications in a number of life domains and these include education, employment, relationships, and leisure. The propensity to recurrent epileptic seizures may curtail someone’s independence and severely impact on quality of life. An acute epilepsy care model may be adequate in treating seizures acutely and may avoid direct medical complications but usually disregards these important aspects of a person’s life. On the other hand, a comprehensive care model provides a holistic approach to the person with the condition.
The delivery of comprehensive care involves a multidisciplinary team whilst acute care is usually based on physician only health delivery, focusing mainly on seizure control. This acute approach may well be adequate for those who have a short lived condition. Comprehensive care often involves voluntary agencies and support groups in addition to the multidisciplinary team. The team delivering comprehensive care usually consists of physicians of various disciplines (neurologists, paediatricians, neurophysiologists, neurosurgeons, psychiatrists, and learning disability specialists), epilepsy specialist nurses, therapists (speech, physio, occupational), social workers as well as counsellors. The team has access to full diagnostic facilities and well as to neurosurgical services. Comprehensive care is proactive and will engage in careful planning of a person’s management path. This is in contrast to acute care which is usually reactive and ad hoc. Comprehensive care is better placed to consider, for instance, the feasibility of epilepsy surgery in an individual person and to plan for it. It may also plan ahead for changes in life status of a person (for example, planned pregnancy). People with well-controlled epilepsy may wish to taper or stop anti-epileptic drug therapy, and this should be the province of comprehensive care. This comprehensive care usually provides full information to the people it serves and will have an open access policy. Comprehensive epilepsy care also involves planned shared care with the primary care provider. There will be a shared-care protocol as well as guidelines for urgent access to the comprehensive care centre.
Despite the intuitive feeling that comprehensive care is better than acute care for people with epilepsy, there is no clear evidence to confirm this. Nevertheless, given the opportunity most people with epilepsy would prefer a comprehensive health delivery approach over the option of ad hoc management. A comprehensive approach usually provides continuity of care which is one of the features that people with epilepsy most appreciate in their assessment of health care delivery.
This presentation will discuss these issues, comparing and contrasting the acute care delivery approach to a full comprehensive care model for people with epilepsy.

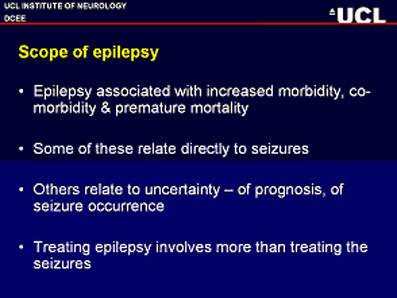
Slide 1: Scope of epilepsy.

Slide 2: Compehensive care.

Slide 3: Comprehensive epilepsy care.

Slide 4: Comprehensive care better?
Source: 8th European Congress on Epiteptology, Satellite Symposium: “Comprehensive Care of Epilepsy in Europe”, Berlin, 20. September 2008 (Medizin und PR Kommunikation).